WHAT IS BRAIN HAEMORRHAGE ?
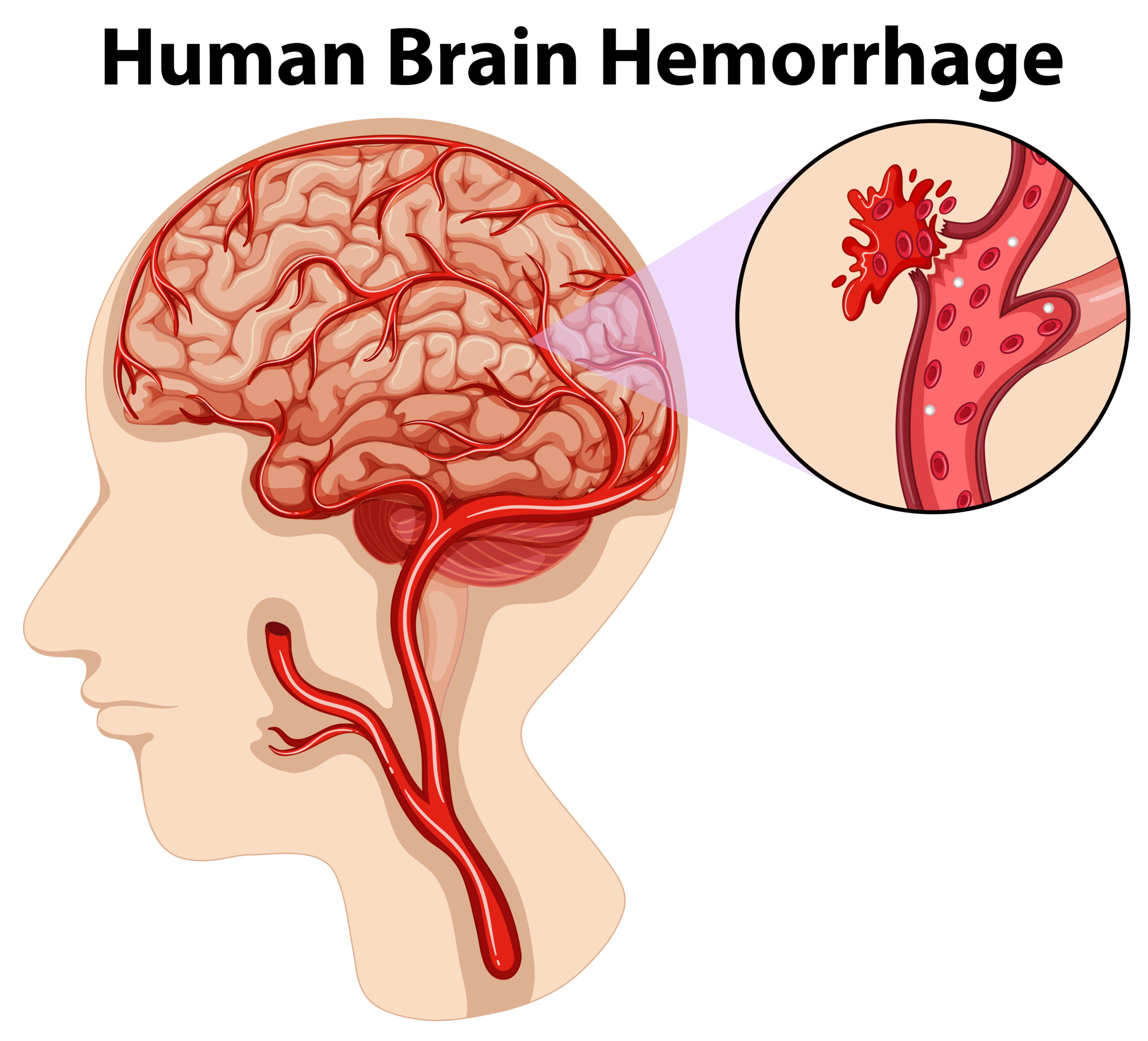
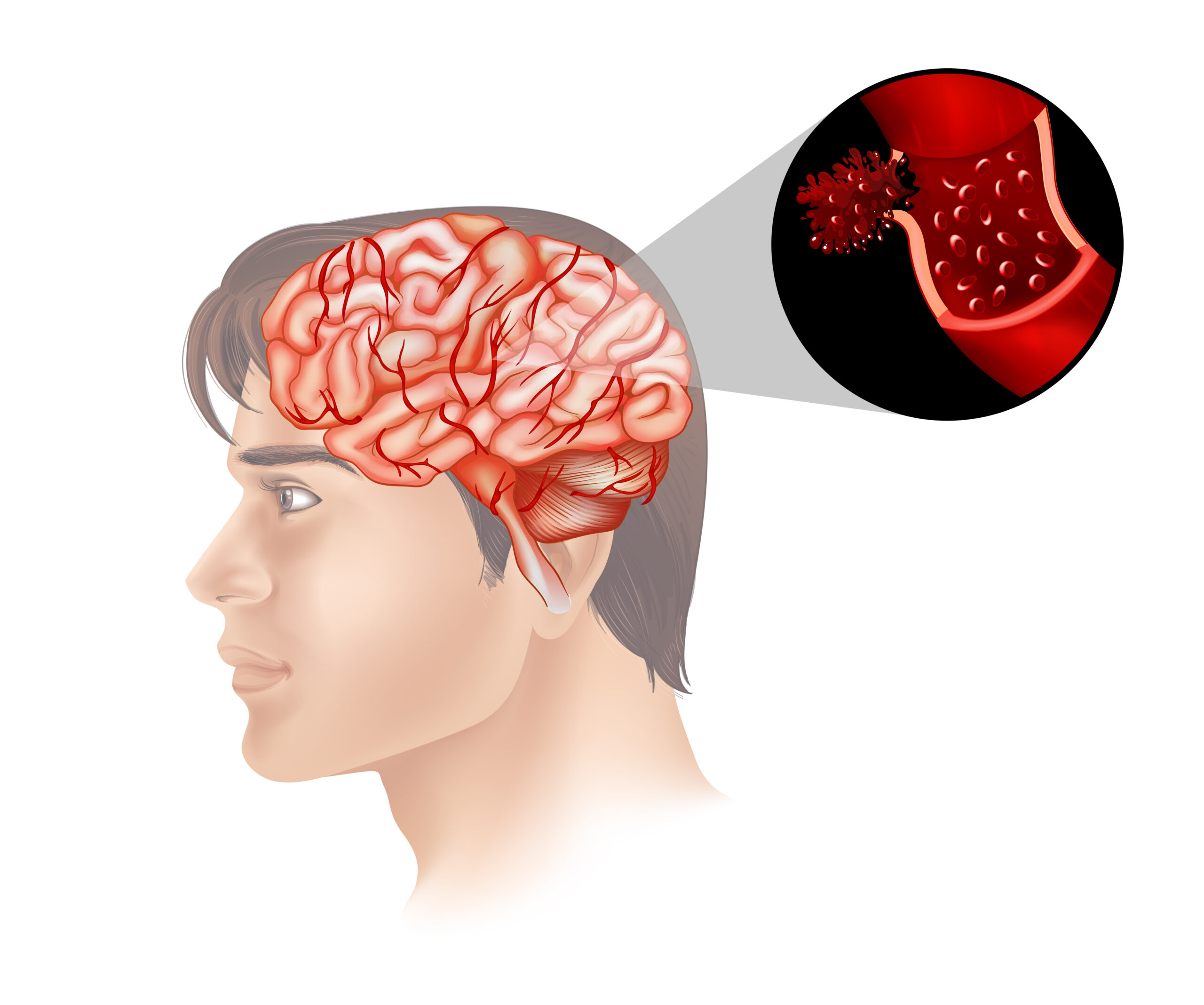
A brain hemorrhage, also known as intracerebral hemorrhage (ICH), is a medical condition in which bleeding occurs within the brain. It can be a life-threatening condition and is a type of stroke. There are several different types of brain hemorrhages, including:
1. Intracerebral (Brain) Haemorrhage (ICH):
Intracerebral haemorrhage (ICH), also known as cerebral bleed, intraparenchymal bleed, and haemorrhagic stroke, is an unexpected bleeding into the brain’s tissues, ventricles, or both. An ICH is a type of bleeding within the skull as well as a type of stroke. Symptoms include headache, one-sided weakness, numbness, tingling, or paralysis, speech difficulties, vision or hearing difficulties, memory loss, attention difficulties, coordination difficulties, balance difficulties, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, and neck stiffness. Symptoms frequently worsen over time. Fever is also rather prevalent.
2. Subarachnoid Haemorrhage (SAH) :
A subarachnoid haemorrhage (SAH) is bleeding into the subarachnoid space—the area surrounding the brain between the arachnoid membrane and the pia mater. Symptoms may include a severe headache with a rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or pain are also relatively common. A small bleed with resolving symptoms occurs in .
3. Epidural Hematoma :
When bleeding occurs between the tough outer membrane surrounding the brain (dura mater) and the skull, this is referred to as an epidural hematoma. Following a head injury, there is frequently loss of consciousness, followed by a temporary recovery of awareness, and then loss of consciousness again. Other symptoms include a headache, confusion, vomiting, and the inability to move some parts of the body. Seizures are one of the possible complications.
4. Subdural Hematoma :
A subdural hematoma (SDH) is a form of haemorrhage in which blood accumulates between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It is frequently caused by tears in the bridge veins that span the subdural region.
Subdural hematomas can create a rise in pressure inside the skull, which can crush and injure sensitive brain tissue. Acute subdural hematomas are frequently fatal. Chronic subdural hepatomas have a better prognosis if they are treated properly.
ALSO READ : Tragic Loss : Wagh Bakri owner , Parag Desai, dies of brain Haemorrhage at 49
WHAT ARE THE CAUSES OF BRAIN HAEMORRHAGE ?
Brain hemorrhages can have various causes, and they often result from the rupture of blood vessels within the brain. Here are some common causes and risk factors for brain haemorrhages:
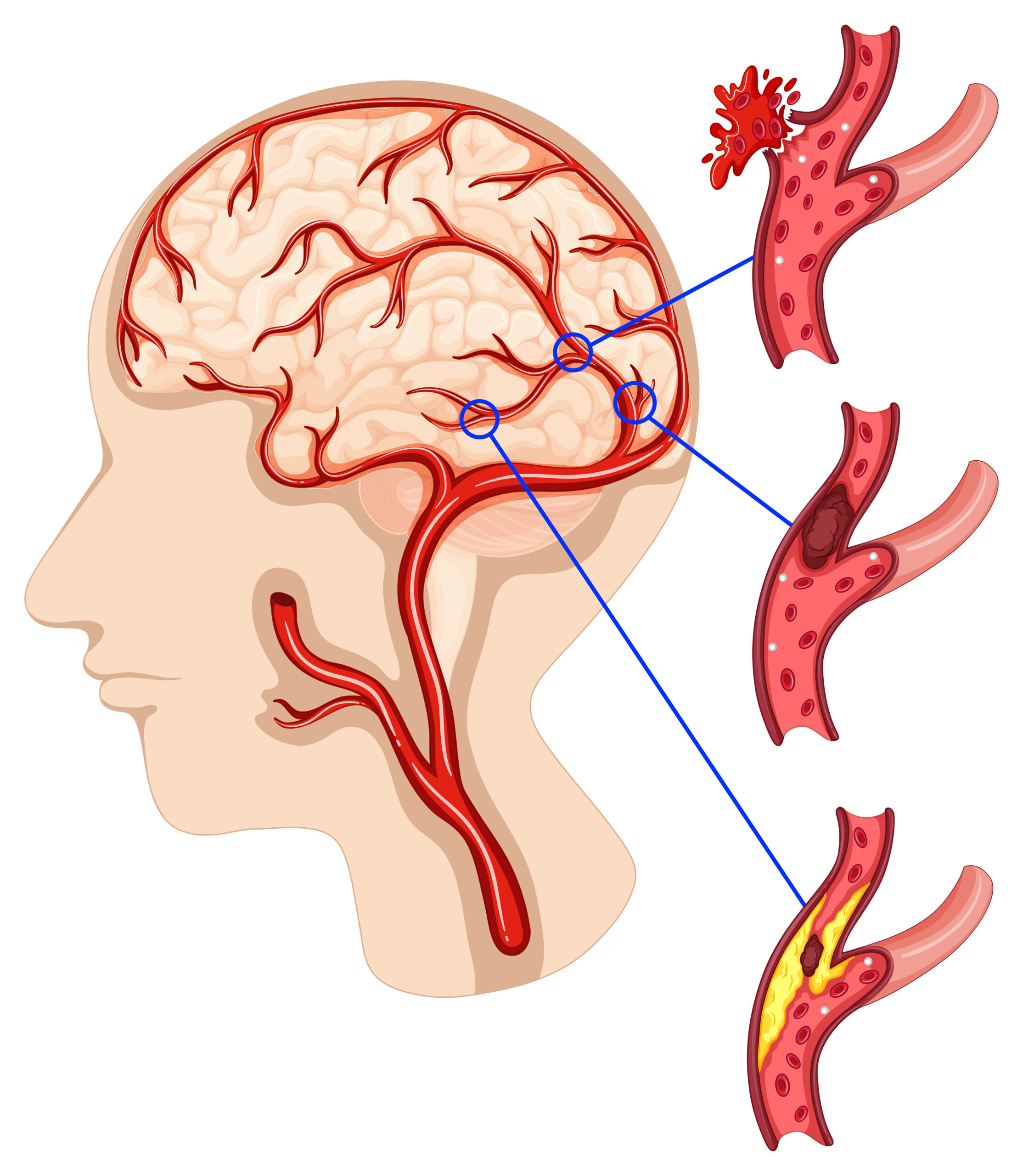
1. Hypertension (High Blood Pressure): Uncontrolled high blood pressure is a leading cause of brain haemorrhages. Chronic high blood pressure can weaken the walls of blood vessels, making them more prone to rupture.
2. Aneurysms: Aneurysms are weak, bulging spots on the walls of blood vessels in the brain. If an aneurysm ruptures, it can cause a significant haemorrhage.
3. Arteriovenous Malformations (AVMs): AVMs are abnormal tangles of blood vessels in the brain that can rupture and lead to bleeding.
4. Head Trauma: Traumatic brain injury, such as a severe blow to the head, can damage blood vessels and cause bleeding within the brain.
5. Brain Tumours: Certain tumours in the brain can put pressure on blood vessels or directly cause them to rupture.
6. Amyloid Angiopathy: This condition involves the buildup of amyloid protein in the walls of blood vessels, increasing the risk of bleeding.
7. Bleeding Disorders: Conditions that affect blood clotting, such as haemophilia or certain medications, can make an individual more susceptible to haemorrhages.
8. Anticoagulant Medications: Blood-thinning medications, like warfarin or aspirin, can increase the risk of bleeding, including brain haemorrhages.
9. Illegal Drug Use: The use of drugs like cocaine or amphetamines can raise blood pressure and increase the risk of a brain haemorrhage.
10. Liver Disease: Liver disorders can lead to clotting problems, making individuals more susceptible to bleeding.
11. Cerebral Venous Sinus Thrombosis: This is a rare condition where blood clots in the brain’s venous sinuses can lead to increased pressure and bleeding.
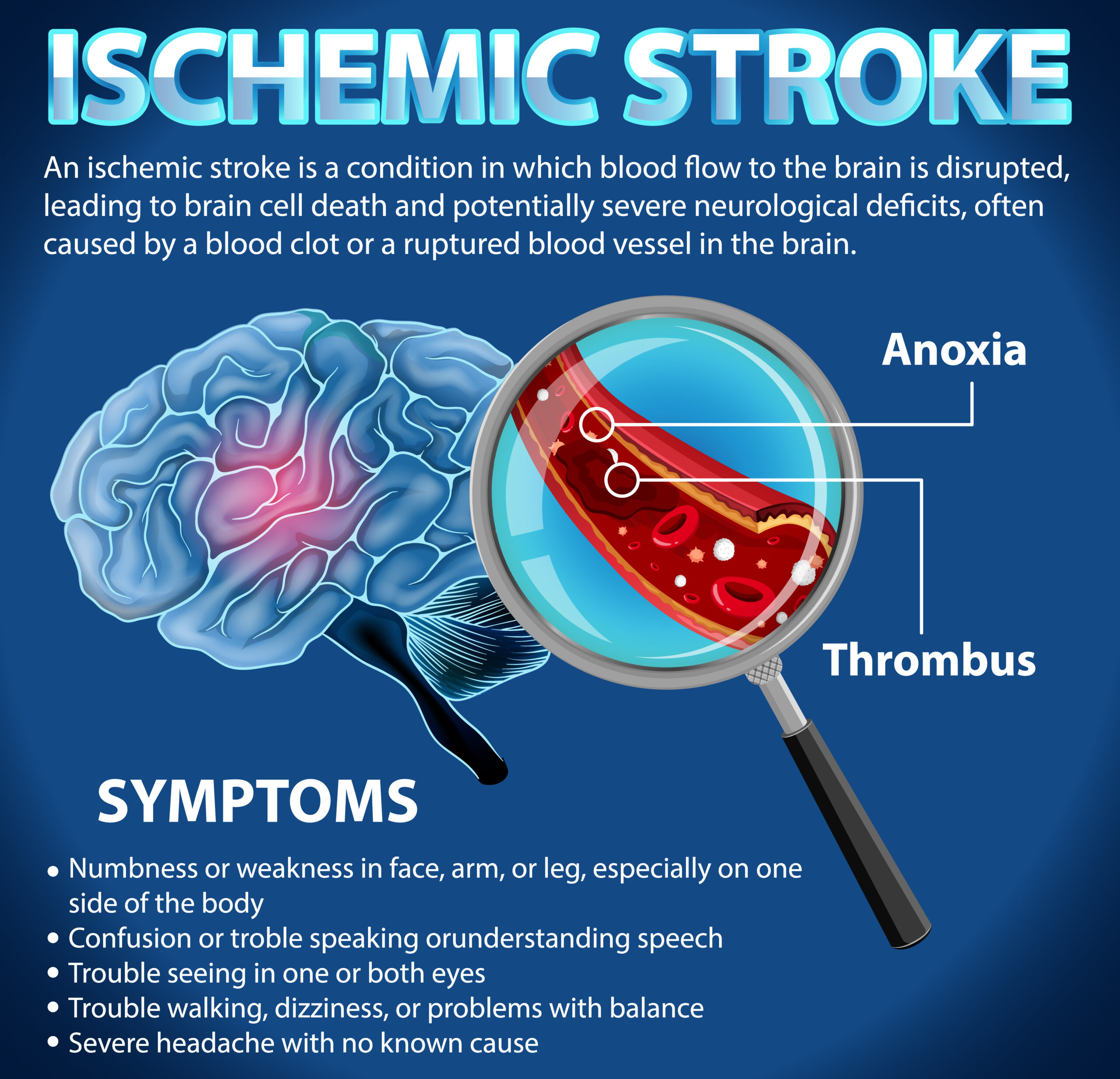
12. Ischemic Stroke: Occasionally, ischemic strokes (caused by blocked blood vessels) can lead to hemorrhagic transformation, where the blocked vessel ruptures and causes bleeding.
13. Age: The risk of brain haemorrhages tends to increase with age, and the elderly are more vulnerable.
It’s important to note that some individuals may have a combination of risk factors that increase their chances of experiencing a brain haemorrhage . Early detection and management of conditions like high blood pressure and the use of anticoagulant medications under medical supervision can help reduce the risk of brain hemorrhages. If you have concerns about your risk factors, it’s advisable to consult with a healthcare professional.
WHAT ARE THE SYMPTOMS OF BRAIN HAEMORRHAGE ?
The symptoms of a brain hemorrhage can vary depending on the location, size, and extent of the bleeding. Common symptoms may include:
1. Sudden Severe Headache: A sudden, extremely severe headache, often described as the “worst headache of one’s life,” is a common symptom of a brain haemorrhage.
2. Nausea and Vomiting: Many people with a brain haemorrhage experience nausea and may vomit.
3. Weakness or Numbness: You may experience weakness or numbness, often on one side of the body. This can affect the face, arm, or leg.
4. Difficulty Speaking: Speech problems, such as slurred speech or difficulty finding the right words, can occur.
5. Vision Changes: Blurred vision, double vision, or other vision problems can be a symptom.
6. Seizures:Some individuals may experience seizures or convulsions.
7. Loss of Consciousness: In severe cases, a brain hemorrhage can lead to loss of consciousness or even coma.
8. Confusion: You may become disoriented or confused, not knowing where you are or what is happening.
9. Balance and Coordination Problems: Difficulty walking, maintaining balance, or coordinating movements is possible.
10. Stiff Neck: In some cases, a stiff neck may be a symptom, although this is more commonly associated with other conditions, such as meningitis.
11. Sensitivity to Light: Increased sensitivity to light (photophobia) may occur.
It’s important to note that the severity and combination of these symptoms can vary. If you or someone you know experiences sudden, severe symptoms like a severe headache or neurological deficits, it is crucial to seek immediate medical attention. A brain hemorrhage is a medical emergency, and early treatment can significantly impact the outcome.
Keep in mind that these symptoms are not exclusive to brain hemorrhages and can be associated with various medical conditions. A medical evaluation by a healthcare professional is essential for an accurate diagnosis and appropriate treatment. Click Here!
CAN BRAIN HAEMORRHAGE CAUSE DEATH ?
Yes, a brain hemorrhage can be a life-threatening condition and can lead to death. The outcome of a brain hemorrhage depends on various factors, including the size of the hemorrhage, its location within the brain, the person’s overall health, and the promptness of medical intervention.
In some cases, a small brain hemorrhage may not lead to immediate death but can result in long-term neurological deficits or disabilities, depending on the part of the brain affected. However, larger hemorrhages or those in critical areas of the brain can lead to severe complications and, if not treated promptly, may result in fatality.
Immediate medical attention is essential when a brain haemorrhage is suspected, as early intervention can significantly improve the prognosis. Treatment may involve surgery to stop the bleeding or relieve pressure on the brain, medications to manage blood pressure and brain swelling, and other medical interventions as needed.
Preventative measures, such as managing risk factors like high blood pressure, seeking timely medical care for conditions that increase the risk of hemorrhage, and avoiding head injuries, can help reduce the likelihood of a brain hemorrhage. If you or someone you know experiences symptoms suggestive of a brain haemorrhage, it is crucial to call for emergency medical assistance.
HOW TO TREAT BRAIN HAEMORRHAGE ?
The treatment of a brain hemorrhage (intracerebral hemorrhage or any other type of bleeding in the brain) is a medical emergency and should be managed by a team of healthcare professionals. The specific treatment approach can vary depending on the cause and extent of the hemorrhage. Here are some general steps and treatments commonly used for brain haemorrhages:
1. Emergency Medical Care: When someone exhibits symptoms of a brain haemorrhage, such as a severe headache, neurological deficits, or loss of consciousness, call 911 or seek immediate medical attention. Quick intervention is crucial to minimize potential damage.
2. Medical Evaluation:The medical team will conduct a thorough evaluation, which may include a physical examination, imaging tests (CT scan or MRI), and other diagnostic procedures to confirm the presence of a brain haemorrhage and determine its location and size.
3. Stabilisation: Patients with brain haemorrhages may require treatment to stabilise vital signs, such as blood pressure and oxygen levels, as these can affect the extent of bleeding and overall brain function.
4. Surgery: Depending on the size and location of the haemorrhage, surgery may be necessary to stop the bleeding or relieve pressure on the brain. Surgical options include craniotomy (removing a portion of the skull to access the brain), aneurysm clipping, and coiling for aneurysm repair.
5. Medications: Medications may be prescribed to manage blood pressure, reduce brain swelling (oedema), and prevent complications. These can include antihypertensive drugs, diuretics, and medications to control seizures.
6. Rehabilitation: After the acute phase, patients often require rehabilitation to regain lost function and improve their quality of life. This may include physical therapy, occupational therapy, speech therapy, and other specialized care.
7. Monitoring: Patients with brain haemorrhages usually require close monitoring in an intensive care unit to assess their condition, manage complications, and adjust treatment as needed.
The specific treatment plan for a brain haemorrhage will depend on individual factors, including the cause of the haemorrhage, the patient’s overall health, and the extent of the damage. It’s important to note that the prognosis for individuals with brain hemorrhages can vary widely, and recovery can be a complex and lengthy process.
The information provided here is for general guidance. The treatment of a brain hemorrhage is a complex medical matter, and decisions should be made by healthcare professionals with expertise in neurology and neurosurgery. If you or someone you know is experiencing symptoms of a brain haemorrhage, seek immediate medical attention.
