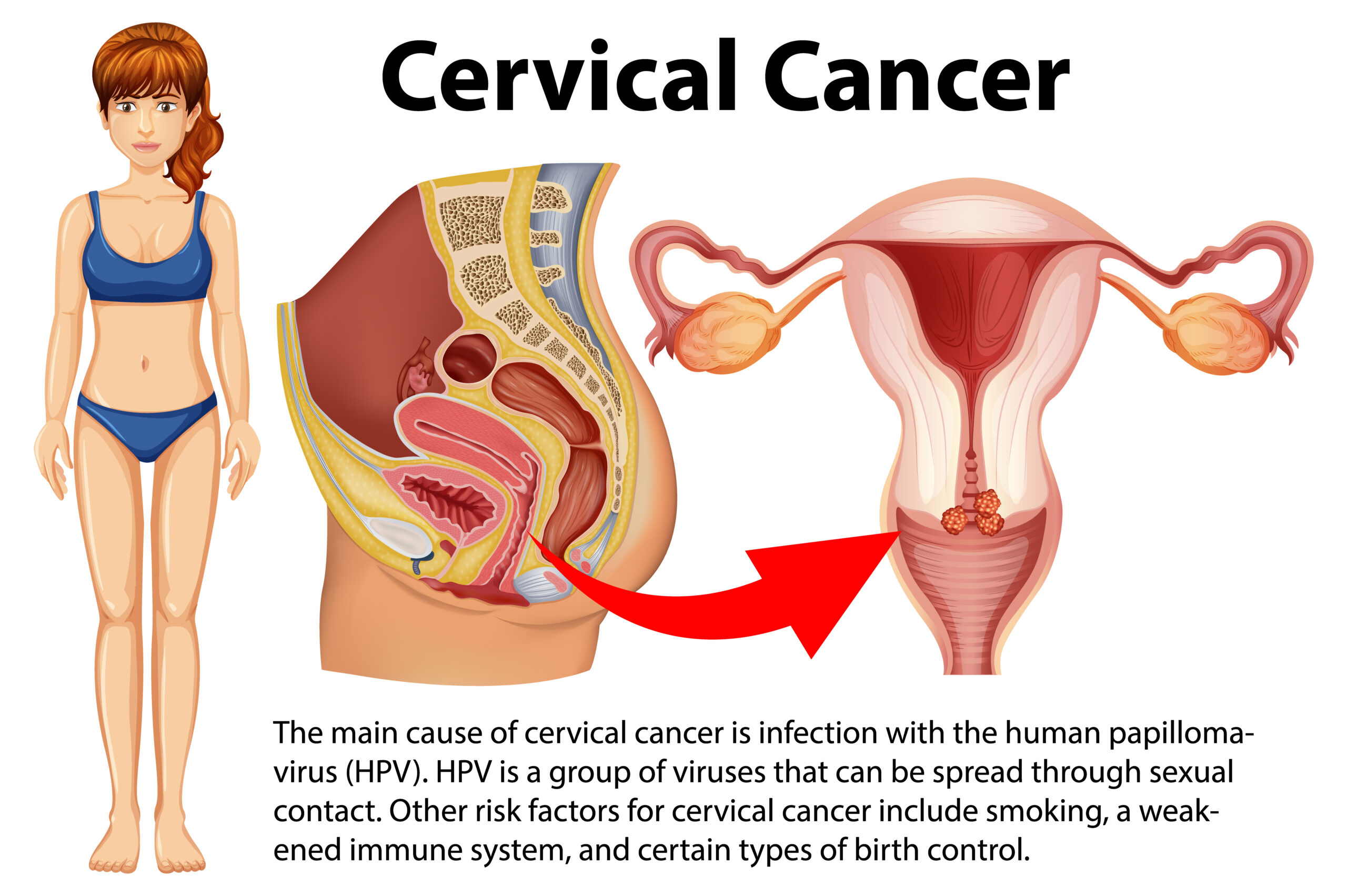
Cervical Cancer
Cervical cancer is a type of cancer that occurs in the cervix, the narrow, lower part of the uterus that connects to the vagina. This cancer typically develops slowly over a period of time and is often caused by persistent infections with certain types of the human papillomavirus (HPV). Here are some key points about cervical cancer.
ALSO READ : “Postpartum Exercise: When and How to Start Safely”
Types of Cervical Cancer
Cervical cancer is primarily classified into two main types:
1. Squamous Cell Carcinoma : This is the most common type of cervical cancer, accounting for about 70-90% of cases. Squamous cell carcinoma develops in the thin, flat cells that line the outer part of the cervix. It usually starts in the transformation zone, where the squamous and columnar cells meet.
2. Adenocarcinoma : Adenocarcinoma makes up the remaining 10-30% of cervical cancer cases. It starts in the glandular cells that line the cervical canal. Adenocarcinoma can be more challenging to detect because it often develops higher in the cervical canal, and it may not be as readily detected in Pap smears as squamous cell carcinoma.
In addition to these two primary types, there are other, less common subtypes of cervical cancer, including:
3. Adenosquamous Carcinoma : This is a less common type of cervical cancer that contains both squamous and glandular cancer cells.
4. Small Cell Carcinoma : This is a rare and aggressive type of cervical cancer that is made up of small, oat-shaped cells.
5. Neuroendocrine Tumors : These are another rare type of cervical cancer that arises from neuroendocrine cells and can be very aggressive.
The treatment and prognosis for cervical cancer may vary depending on the specific type, its stage at diagnosis, and other factors. Regular screenings and early detection are crucial in improving outcomes for individuals with cervical cancer. If you have concerns about cervical cancer or related health issues, it’s important to consult with a healthcare professional for a proper diagnosis and guidance on treatment options. Click Here!

Causes of Cervical Cancer
Cervical cancer is primarily caused by persistent infection with certain types of the human papillomavirus (HPV). HPV is a group of sexually transmitted viruses, and some of its high-risk types can lead to the development of cervical cancer. Here are the primary causes and risk factors associated with cervical cancer:
1. HPV Infection : The most significant risk factor for cervical cancer is infection with high-risk types of HPV, particularly HPV-16 and HPV-18. These types of HPV are responsible for most cases of cervical cancer. HPV is very common and is usually transmitted through sexual contact. In most cases, the body’s immune system clears the virus within a couple of years. However, in some cases, the virus can persist and lead to precancerous changes and eventually cervical cancer.
2. Smoking : Smoking is a known risk factor for cervical cancer. Women who smoke are more likely to develop cervical cancer than non-smokers. The harmful chemicals in tobacco smoke may make the cervical cells more vulnerable to the effects of HPV.
3. Weakened Immune System : A weakened immune system, whether due to conditions like HIV/AIDS or immunosuppressive medications, can increase the risk of developing cervical cancer because the body may have more difficulty fighting off HPV infections.
4. Early Sexual Activity : Beginning sexual activity at an early age may increase the risk of HPV infection, as the immune system is less developed in younger individuals.
5. Multiple Sexual Partners : Having multiple sexual partners can increase the risk of HPV exposure and infection.
6. History of Sexually Transmitted Infections (STIs) : Previous or current STIs, such as chlamydia or gonorrhea, may increase the risk of cervical cancer.
7. Family History : Although less common, there may be a genetic predisposition to cervical cancer in some families.
It’s important to note that having one or more of these risk factors doesn’t mean that someone will develop cervical cancer. Many women with these risk factors never develop the disease, and many cases of cervical cancer occur in women without these risk factors. Regular cervical cancer screenings, such as Pap tests and HPV tests, are essential for early detection and prevention. Additionally, HPV vaccines are available to protect against some of the high-risk types of HPV that can lead to cervical cancer.
Signs and Symptoms of Cervical Cancer

Cervical cancer may not cause noticeable symptoms in its early stages. However, as the cancer progresses, the following signs and symptoms may become more apparent:
1. Abnormal Vaginal Bleeding : This is one of the most common and important symptoms of cervical cancer. It may include:
– Bleeding between periods.
– Bleeding after sexual intercourse.
– Bleeding after menopause (when menstrual periods have stopped).
2. Unusual Vaginal Discharge : Women with cervical cancer may experience increased vaginal discharge that may be bloody, watery, or foul-smelling.
3. Pelvic Pain : This pain may occur in the lower abdomen or pelvis, and it can range from mild to severe.
4. Pain During Sexual Intercourse : Some women with cervical cancer may experience discomfort or pain during sexual activity.
5. Painful Urination : Cervical cancer can sometimes cause pain or discomfort during urination, but this is less common.
6. Pain in the Legs or Back : In advanced stages of cervical cancer, the cancer may spread to other areas, causing pain in the legs or lower back.
It’s important to note that these symptoms can be caused by various other conditions, and having these symptoms does not necessarily mean you have cervical cancer. However, if you experience any of these signs and they persist or are unusual for you, it’s essential to see a healthcare provider for evaluation and appropriate testing.
Regular cervical cancer screenings, including Pap tests and HPV tests, are vital for early detection and can often find precancerous changes before they progress to cancer. Early detection can greatly improve the chances of successful treatment. If you have concerns or risk factors related to cervical cancer, discuss them with your healthcare provider.
Diagnosis of Cervical Cancer
The diagnosis of cervical cancer typically involves a series of tests and procedures to confirm the presence of cancer, determine its stage, and plan appropriate treatment. Here are the key steps involved in diagnosing cervical cancer:
1. Pelvic Examination : A pelvic examination is often the first step. The healthcare provider examines the cervix, vagina, and surrounding areas for any unusual changes or abnormalities. They may also use a speculum to open the vagina for a clearer view.
2. Pap Test (Pap Smear) : A Pap test is a routine screening test to detect abnormal cervical cells. During this test, a sample of cells is collected from the cervix and examined for any precancerous or cancerous changes. If abnormal cells are detected, further testing is usually required.
3. HPV Test : In addition to or in combination with the Pap test, an HPV test may be performed to identify high-risk types of the human papillomavirus (HPV) that are associated with cervical cancer.
4. Colposcopy : If the Pap test or HPV test indicates abnormal results, a colposcopy may be performed. During this procedure, a special magnifying instrument (colposcope) is used to closely examine the cervix. If suspicious areas are identified, a biopsy may be taken.
5. Cervical Biopsy : A biopsy is the definitive way to diagnose cervical cancer. It involves the removal of a small sample of cervical tissue for examination under a microscope. The type of biopsy can include:
– Punch biopsy : A small piece of tissue is removed using a special instrument.
– Cone biopsy (conization) : A cone-shaped piece of tissue is removed, and it is often used for more extensive sampling.
– Endocervical curettage : This involves scraping tissue from the cervical canal.
6. Imaging Tests : To determine the extent and stage of the cancer, imaging tests such as CT scans, MRI scans, or PET scans may be performed to check for the spread of cancer to nearby lymph nodes or other organs.
7. Lymph Node Biopsy : If there is concern that the cancer has spread to nearby lymph nodes, a biopsy of these nodes may be necessary to confirm the presence of cancer cells.
The results of these diagnostic tests are used to determine the stage and extent of cervical cancer, which is crucial in planning appropriate treatment. Cervical cancer is typically staged from 0 to IV, with higher stages indicating more advanced cancer. Once the diagnosis and staging are complete, healthcare providers will work with the patient to develop a treatment plan that may include surgery, radiation therapy, chemotherapy, or a combination of these treatments. Early diagnosis and treatment can greatly improve the chances of successful outcomes in cervical cancer.
Surgical Interventions of Cervical Cancer
Surgical interventions are one of the primary treatment options for cervical cancer, particularly in the early stages of the disease. The type of surgery recommended depends on the stage and extent of the cancer, the patient’s overall health, and other individual factors. Here are some common surgical procedures for cervical cancer:
1. Cone Biopsy (Conization) : In cases where the cancer is very early and localized, a cone biopsy may be performed. This procedure involves removing a cone-shaped piece of tissue from the cervix. It can also serve as a diagnostic tool, as the removed tissue is examined under a microscope to confirm the presence of cancer.
2. Lymph Node Dissection (Lymphadenectomy) : If there is concern that the cancer has spread to nearby lymph nodes, a lymph node dissection may be performed. This involves removing and examining lymph nodes to determine if cancer cells have spread.
3. Radical Hysterectomy : In this procedure, the cervix, the upper part of the vagina, and the uterus are removed, along with the surrounding tissues and lymph nodes. It is often recommended for early-stage cervical cancer.
4. Radical Trachelectomy : This surgery is a fertility-sparing option for young women with early-stage cervical cancer who wish to preserve their ability to have children. It involves removing the cervix and the upper part of the vagina while leaving the uterus intact.
5. Pelvic Exenteration : For more advanced cases of cervical cancer, especially when the cancer has spread beyond the cervix, pelvic exenteration may be necessary. This extensive procedure involves removing the cervix, uterus, vagina, nearby lymph nodes, and other pelvic organs, such as the bladder or rectum.
6. Minimally Invasive Surgery : Minimally invasive approaches, such as laparoscopic or robotic-assisted surgery, are increasingly used for some surgical procedures, including radical hysterectomy. These techniques involve smaller incisions and can offer quicker recovery times and shorter hospital stays.
The choice of surgery depends on factors like the stage of cancer, the patient’s age, desire for fertility preservation, overall health, and the surgeon’s expertise. After surgery, patients may need additional treatments such as radiation therapy, chemotherapy, or a combination of both to ensure that any remaining cancer cells are treated. It’s crucial for patients to discuss their options, risks, and benefits with their healthcare team to make informed decisions about their cervical cancer treatment.
Medical Interventions of Cervical Cancer
Medical interventions for cervical cancer typically involve the use of radiation therapy, chemotherapy, targeted therapy, and immunotherapy. These treatments may be used alone or in combination, depending on the stage and extent of the cancer, as well as the patient’s overall health. Here are the main medical interventions for cervical cancer:
1. Radiation Therapy :
– External Beam Radiation : This is the most common type of radiation therapy for cervical cancer. It involves directing high-energy X-rays or other particles at the tumor from outside the body.
– Internal Radiation (Brachytherapy) : In brachytherapy, radioactive sources are placed inside or very close to the tumor. This method delivers a high dose of radiation directly to the cancer while minimizing exposure to surrounding healthy tissues.
2. Chemotherapy :
– Chemotherapy involves the use of drugs that kill or slow the growth of cancer cells. It can be administered intravenously (IV) or orally.
– Often, chemotherapy is used in combination with radiation therapy to enhance its effectiveness (chemoradiation).
3. Targeted Therapy :
– Targeted therapies are drugs that target specific molecules or pathways involved in the growth and spread of cancer cells. Bevacizumab is an example of a targeted therapy used in the treatment of advanced cervical cancer.
4. Immunotherapy :
– Immunotherapy drugs work by boosting the body’s immune system to recognize and attack cancer cells. Pembrolizumab and nivolumab are examples of immunotherapy drugs approved for advanced cervical cancer.
5. Clinical Trials :
– Participation in clinical trials may be an option for some patients. These trials investigate new treatments, combinations of treatments, and novel therapies to improve outcomes for individuals with cervical cancer.
The specific treatment plan for cervical cancer depends on factors such as the stage of cancer, the type of cervical cancer, the patient’s overall health, and the response to treatment. Treatment decisions are often made in collaboration with a multidisciplinary team of healthcare professionals, including oncologists, radiation oncologists, and surgeons.
It’s important for patients to discuss the potential benefits and side effects of each treatment option with their healthcare team to make informed decisions about their cervical cancer treatment. Early-stage cervical cancer is often curable with the right treatment, while advanced-stage cancer may require a combination of therapies to manage and control the disease.
Rehabilitative Interventions of Cervical Cancer

Rehabilitative interventions for cervical cancer aim to improve the physical, emotional, and functional well-being of individuals who have undergone treatment for cervical cancer. These interventions help patients recover from the effects of cancer and its treatment and enhance their quality of life. Here are some rehabilitative interventions and support services for cervical cancer survivors:
1. Physical Rehabilitation :
– Pelvic Floor Rehabilitation : Many women who have had cervical cancer treatment, including surgery and radiation, may experience pelvic floor dysfunction. Physical therapists can provide exercises and interventions to improve pelvic floor strength and function.
– Lymphedema Management : Some individuals may develop lymphedema, a swelling in the legs or lower body due to lymph node removal or radiation therapy. Lymphedema therapists can offer techniques to manage this condition and reduce swelling.
-Pain Management: Patients who experience pain after treatment can benefit from pain management strategies, including medications, physical therapy, and complementary therapies like acupuncture.
2. Psychosocial Support :
– Counseling and Support Groups : Psychosocial support services, such as individual counseling and group therapy, can help individuals cope with the emotional and psychological challenges of cancer diagnosis and treatment.
– Sexual Health Counseling : Many women experience changes in their sexual health and intimacy after cervical cancer treatment. Counselors can provide guidance and support to address these issues.
– Mind-Body Practices : Techniques like meditation, mindfulness, and yoga can help patients manage stress and improve emotional well-being.
3. Dietary and Nutritional Support :
– Registered dietitians can provide guidance on nutrition and dietary strategies to manage potential side effects of treatment and promote overall health.
4. Palliative Care and Pain Management :
– Palliative care specialists can assist in managing pain and improving the overall quality of life, particularly in advanced cases of cervical cancer.
5. Speech and Swallowing Therapy : In cases where radiation therapy impacts the throat or esophagus, speech and swallowing therapists can help patients regain their ability to eat and communicate comfortably.
6. Reconstructive Surgery : For women who have undergone extensive surgical procedures, reconstructive surgery may be an option to improve the appearance and function of the pelvic area.
7. Fertility Preservation and Family Planning : For women who wish to have children in the future, fertility preservation options, such as egg freezing or embryo banking, can be explored before undergoing cervical cancer treatment.
8. Survivorship Care Plans : These personalized plans outline the long-term follow-up and healthcare needs of cervical cancer survivors, including surveillance for recurrence and management of potential long-term side effects.
It’s essential for individuals affected by cervical cancer to work with a multidisciplinary healthcare team that includes oncologists, physical therapists, mental health professionals, and other specialists to develop a comprehensive rehabilitation and support plan tailored to their unique needs and goals. Rehabilitation and support services can significantly contribute to a better quality of life for cervical cancer survivors.

Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
I appreciate your creativity and the effort you put into every post. Keep up the great work!
I like the efforts you have put in this, regards for all the great content.